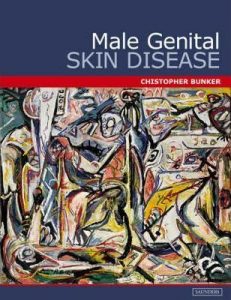
Male Genital Skin Disease
Christopher B Bunker
Atlas organised by differential diagnosis of clinical presentations of male genital skin disease. It includes the important entities of psoriasis, lichen sclerosus and penile intraepithelial neoplasia.
Since writing this book 15 years ago a number of advances have occurred that make some of the text redundant, inaccurate or incomplete. The most important progress has been made in lichen sclerosus and penile intraepithelial neoplasia (discussed below).
This is an eBook version of the book previously published in 2004 with this original cover reviewed here
Lichen sclerosus (LSc).
My observations, experience, research and clinical outcomes over the last decade and a half indicate that LSc is due to occluded exposure of a susceptible balanopreputial epithelium to urine. The urinary exposure comes about because of urinary micro-incontinence or dribbling. This is because on meticulous inspection patients are found to have an embryogenic forme fruste of hypospadias or because distal naviculomeatal and urethral urodynamics are disturbed by urological interventions for the investigation of other diseases, other dermatoses, STDs, or genital piercing. The naviculomeatal dysfunction is worsened by the progression of the LSc. Increasingly in some circumcised men LSc occurs because obesity leads to the development of a pseudo- or neo-foreskin and occlusion of dribbled urine is able to occur. Understanding the role of urine is crucial to prevention, diagnosis, treatment and prognosis.
Penile intraepithelial neoplasia (PeIN)/carcinoma in situ (CIS).
This remains a confusing field because of inconsistent use of terminology and changing definitions. An important development has been the appreciation of the dichotomy between differentiated (LSc-related) and undifferentiated (HPV-driven PeiN) as in the vulva. However, increasingly, compounding overlap situations are clinically encountered especially in acquired immunosuppresion (HIV, transplant patients and biologics). Adjunctive post-exposure HPV vaccination is advocated me and my colleagues in the management of differentiated HPV-related but remains contentious.